Fires, bad air quality and COVID-19: a triple threat for those with lung problems
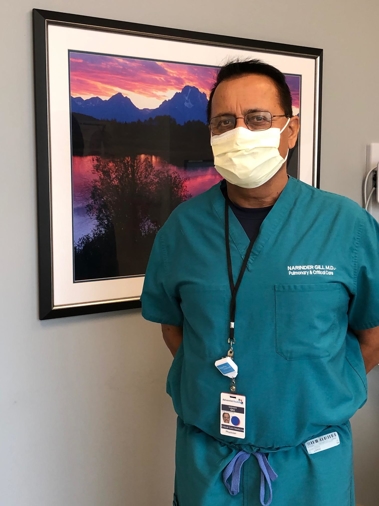
In his more than 35 years of practicing medicine, Dr. Narinder Gill, board-certified pulmonologist at the Adventist Health Lung Care Center, says he’s never seen anything like we’re experiencing now.
Bad air quality from the wildfires raging across California, combined with a national pandemic and harvesting season in the Central Valley, is causing concerns for people who suffer from respiratory problems.
“Smoke is a trigger for people with asthma, allergies, chronic obstructive pulmonary disease and many other lung conditions,” says Dr. Gill. “The problem occurs when these triggers cause a flare-up of symptoms that could lead to life-threating conditions, including pneumonia.”
Dr. Gill says each person has their own trigger. Some might be sensitive to smoke or pollens, while others might be sensitive to extreme heat or cold. However, some people’s lungs can tolerate the conditions without reacting, which could allow them to get by unscathed, until the smoke clears.
How to stay safe
Measures that can help ease flare ups:
1. Staying indoors
2. Using an inhaler consistently, if you have asthma or COPD
3. Visiting the doctor or emergency room, if symptoms worsen
4. Staying hydrated
Measures that can help residents escape bad air:
1. Staying indoors
2. Closing windows
3. Turning on the air conditioner
4. Avoiding use of swamp coolers, if possible
5. Placing HEPA filters inside homes
6. Using an air purifier
7. Using a cool mist humidifier
8. Turning on sprinklers to settle pollution and dry air
9. Wearing a mask
Symptoms
Flare-ups lead to coughing, which also happens to be the main symptom of COVID-19. So how can you determine whether your coughing is due to bad air or COVID-19?
“Symptoms can be overlapping and deceiving,” says Dr. Gill. “The only way you can differentiate whether the coughing is due to allergies, asthma or COVID, is by clues.”
Clues it’s COVID-19
Dr. Gill explains that if someone doesn’t have a history of respiratory problems, but has a cough, fever, shortness of breath, or any other symptom related to COVID-19, they should suspect COVID-19. A COVID-19 symptom checker is available at AdventistHealth.org.
Clues it’s Asthma
If someone has a history of asthma and experiences similar symptoms every year during this time, they should not suspect COVID-19. If symptoms decrease with the use of an inhaler, the person would know the breathing trouble is due to asthma, since COVID-19 symptoms won’t improve with an inhaler.
Clues it’s Allergies
Allergies affect different areas of the breathing tubes but are limited to the nose and affect the nasal area and upper airways. Additional symptoms of allergies include itchy eyes and an itchy throat.
Wearing a mask can help
Dr. Gill assures that people with respiratory problems don’t have to fear breathing trouble, if they wear a mask.
“Masks do not block air,” he says. “When you wear a mask, you’re inhaling air with a filter in between, which can filter smoke, pollution and COVID-19.”
Harvesting season
Fall is approaching, which means harvesting season. This is the time when crops are gathered from fields. Typically, tractors are used, which create large clouds of dust. The dust, combined with smoke, can lead to an uncomfortable situation for those with respiratory problems.
Seeking care
With the combination of bad air and coughing bouts, Dr. Gill expects to see more patients arrive to the Lung Care Center, which reopened in June. The Lung Care Center is staffed by three physicians who are specially trained in pulmonary medicine.
The Lung Care Center has the same safety precautions in place, as all facilities across Adventist Health in the Central Valley, to protect patients from COVID-19. Such measures include requiring masks before entering the building, temperature screenings, asking about symptoms and physical distancing in waiting areas.
Patients may seek care at the Lung Care Center with a referral from their primary care provider.
More information may be found at HanfordLungCare.com.




